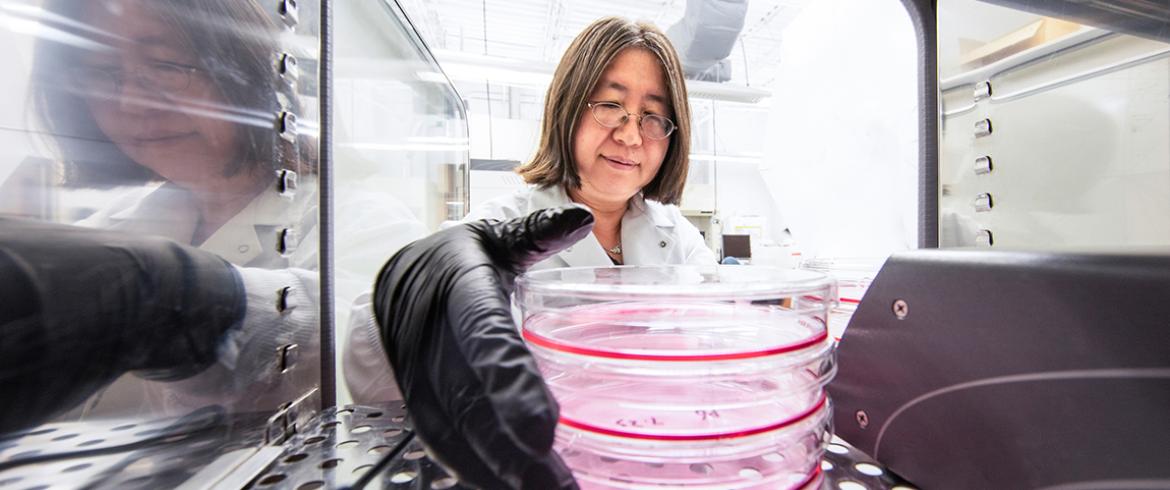
Yan Li, associate professor in the Department of Chemical & Biomedical Engineering at the FAMU-FSU College of Engineering, pulls stem cell cultures from the incubator in her lab. (M Wallheisier/FAMU-FSU College of Engineering)
Florida State University researchers have developed a promising strategy for producing therapeutic particles in stem cells, work that could help patients with neurological diseases such as stroke or multiple sclerosis.
The technique developed by researchers from the FAMU-FSU College of Engineering and FSU College of Medicine combines three-dimensional growing platforms with a wave motion. The research was published in the Journal of Extracellular Vesicles.
The particles released by cells — known as extracellular vesicles — are chemical messengers that affect the behavior of cells. They can be used to carry medicine to target organs within the body. Improving the production and effectiveness of these particles is a major field of research.
The FSU researchers combined two techniques for producing these particles. The first was to grow stem cells within a 3D culture rather than a two-dimensional one. The second was to suspend the growing cells on the platform that was rocked back and forth in a gentle motion, producing small waves that helped deliver oxygen, glucose and other nutrients to the cells. Their combined method led the stem cells to produce twice as many particles as those grown in a 2D platform.
“Just like a river’s flow will move more matter than a static lake, our use of dynamic waves in the growth of these stem cells will deliver more nutrients to the cells than if they were just suspended in the culture media,” said senior author Yan Li, an associate professor of chemical and biomedical engineering in the FAMU-FSU College of Engineering.
The extracellular vesicles from the 3D-grown stem cells also exhibited more therapeutic properties than the 2D version. They contained higher amounts of micro ribonucleic acid (RNA) molecules that help protect the brain against neurological diseases and in cases of spinal cord injury, and they also had more anti-inflammatory proteins.
The work also could help treat patients with neurological diseases such as multiple sclerosis, stroke and Alzheimer’s disease. Those diseases disrupt the cell-to-cell interactions needed to repair the brain. Extracellular vesicles harvested from manufactured stem cells mimicking human neural cells could provide the molecules that tell a patient’s damaged cells to begin repairing.
“The vesicles contain a lot of micro-RNAs and proteins, and those change how the cells behave,” Li said. “They don't speak or write a word, but they deliver signals. They put out what are like packages — the particles. They send those, other cells receive them, and they change what those cells do. The engineering approach is to make the cells deliver the desired signals.”
This work was supported by the National Science Foundation, the Florida Department of Health’s Ed and Ethel Moore Alzheimer's Disease Research Program, the National Institutes of Health and Synergy Biologics, LLC.